Adolescent Preventing Harm & Protecting Patients Policies
Patient Information & Aftercare Policy (Age-Appropriate)
HAUS OF ÄSTHETIK
Patient Information & Aftercare Policy (Age-Appropriate)
Effective Date: 1st April 2025
Review Date: 1st April 2026
Approved By: Clinical Governance Lead
Version: 1.0
1. Purpose
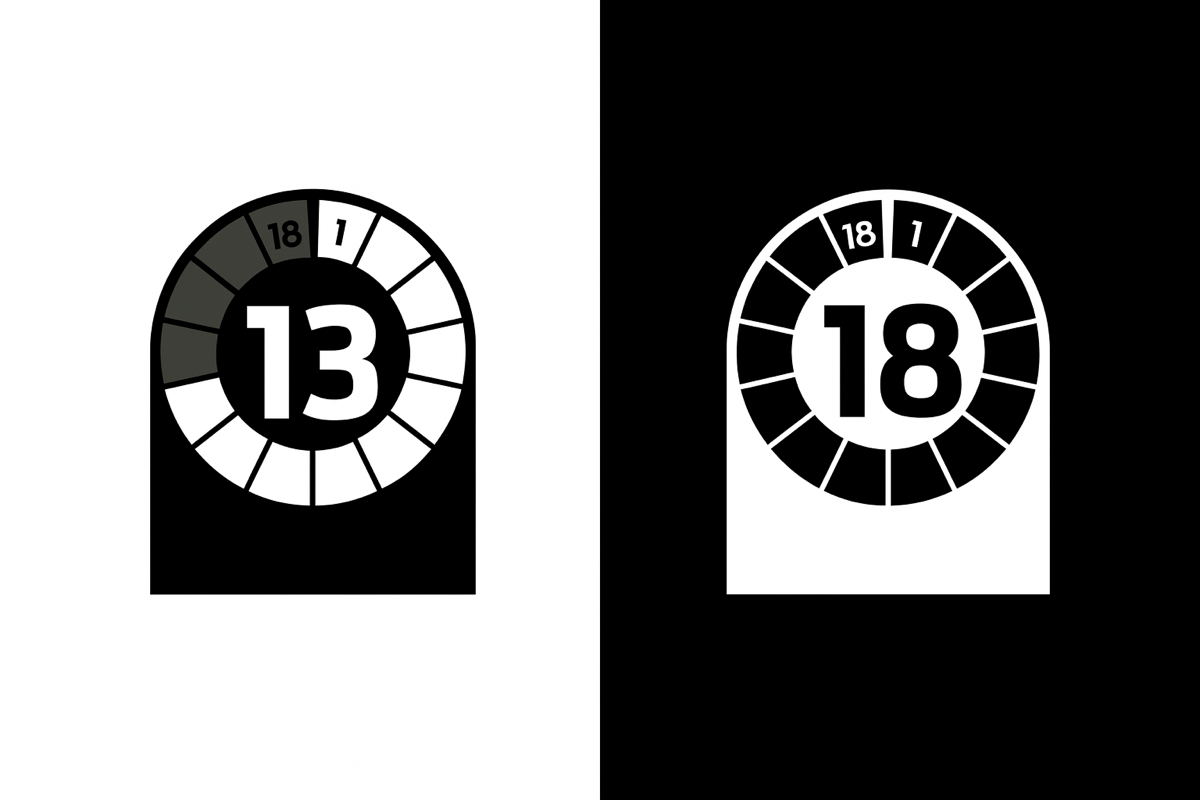
This policy ensures that all patient-facing materials – including pre-treatment information, consent guidance, and aftercare instructions – are tailored appropriately for the age, cognitive ability, and social context of the patient. It ensures safe, informed participation in clinical care, particularly for young people aged 13–17.
It supports our regulatory duties under:
-
CQC Regulation 9: Person-Centred Care
-
CQC Regulation 17: Good Governance
-
Gillick Competence and Fraser Guidelines
-
The Children Act 1989 & 2004
-
Save Face Standards for Patient Information
-
Professional guidance from NMC, GMC and HCPC
2. Scope
This policy applies to:
• All under-18 patients (aged 13–17) receiving approved treatments within the scope of the clinic
• Their parents, carers, and legal guardians
• Clinical and administrative staff providing consultation, consent, or aftercare support
• Third-party materials sourced from manufacturers or regulatory-approved suppliers
3. Principles
-
Informed Consent Requires Comprehension: Information must be presented in a way that the patient can understand, based on age and maturity.
-
Parental Involvement: Where Gillick competence is not clearly established, the consent process must involve a parent or legal guardian.
-
Manufacturer Guidance Compliance: All clinical materials and aftercare literature must align with documentation, usage instructions, and contraindications provided by the manufacturer, including any specific age restrictions or considerations.
-
Cultural and Social Sensitivity: Materials will reflect diverse patient experiences and avoid technical jargon, while acknowledging typical teenage behaviour and daily routines.
4. Age-Adjusted Patient Literature
For patients aged 13–17, patient literature will be:
• Simplified linguistically: Plain English, short sentences, no medical jargon
• Visually accessible: Use of icons, diagrams, and product illustrations
• Treatment-specific: Only relating to permitted treatments (e.g. chemical peels for acne/post-acne scarring)
• Shared in print and digital format: Accessible at the clinic or via secure electronic communication
• Consistent with manufacturer literature: Content must be cross-checked against product SPCs, IFUs, and safety information specific to the patient’s age cohort
Example adaptation:
-
Retain product-specific pH values, application durations, or risk of photosensitivity
-
Translate into relatable terms: e.g., “Don’t pick at your skin after the peel, even if it flakes”
-
Highlight frequency limits: “You’ll only have this treatment every 2–4 weeks, and only if your skin has fully healed.”
5. Aftercare Considerations for Young People
When providing aftercare instructions for patients aged 13–17, staff must ensure that materials and verbal advice account for:
-
School attendance: Timetabling treatments to avoid school photos, exams, or sports
-
Sports activities: Advice around sweating, friction (helmets, pads), and avoiding contamination post-treatment
-
Use of makeup or skincare products: Clear timelines for when non-comedogenic products can be resumed
-
Peer influence and social media behaviour: Guidance around sharing before/after images, picking at skin, or misusing treatment
-
Parent/carer involvement: Aftercare advice must be shared with the legal guardian unless the patient is Gillick competent and declines
-
Contraindicated behaviours: No sunbeds, exfoliants, acne “home remedies,” or over-the-counter actives unless approved by the clinician
-
Emergency contact instructions: Clear, printed instructions for what to do if there is pain, swelling, peeling, or allergic reaction
6. Consent Materials and Record-Keeping
• All treatment documentation must be designed for dual consent (patient and parent, where applicable).
• Consent forms must include a section verifying that the patient received age-adjusted information.
• Copies of the literature given to the patient must be logged in their treatment record.
• Digital platforms such as Insync Consent will retain digital ID, signed consent, and treatment-specific aftercare records.
7. Staff Training
• Staff delivering care to under-18 patients must receive mandatory training in communication with young people, safeguarding, and Gillick competence.
• Staff must know how to explain clinical terminology using analogies or visual tools suitable for teenagers.
• Team members must be familiar with product leaflets and manufacturer guidance for all treatments offered to patients under 18.
8. Monitoring & Compliance
• Patient feedback will be reviewed annually to ensure that materials are accessible and age-appropriate.
• The Clinical Governance Lead will audit patient literature every 12 months or sooner if treatment changes occur.
• Non-compliance with this policy will result in a review of practice standards and, where necessary, disciplinary procedures.
Signed:
Clinical Governance Lead
Date: 1st April 2025
