Adolescent Preventing Harm & Protecting Patients Policies
Safeguarding Disclosure & Parental Attendance Protocol
HAUS OF ÄSTHETIK
Safeguarding Disclosure & Parental Attendance Protocol
Effective Date: 1st April 2025
Review Date: 1st April 2026
Author: Clinical Governance Lead
Approved By: Managing Director
Version: 1.0
1. Purpose
This protocol sets out the requirements for parental attendance and consent during consultations and treatment planning for patients under 18 years of age, with a specific focus on safeguarding disclosure, Gillick competence, and informed decision-making. It ensures compliance with:
-
Children Act 1989 & 2004
-
Working Together to Safeguard Children (HM Gov, 2018)
-
CQC Regulation 13 – Safeguarding
-
NMC Code of Conduct (2018)
-
GMC 0–18 Years: Guidance for all doctors
-
Gillick v West Norfolk & Wisbech AHA [1985] UKHL 7
2. Scope
This protocol applies to:
-
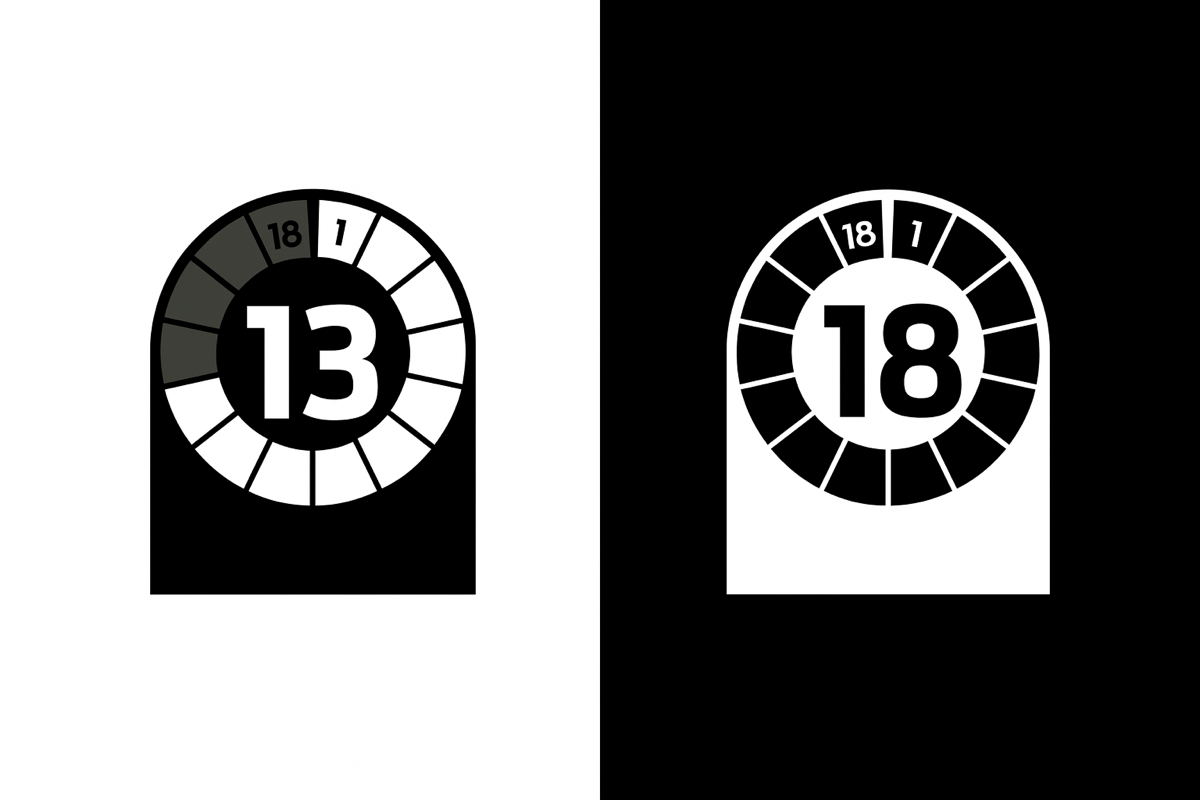
All clinic staff involved in the care or treatment of individuals aged 13 to 17
-
All patients under 18 attending for acne or post-acne scarring treatments
-
All clinical consultations involving under-18s where safeguarding, disclosure, or consent is required
3. Key Principles
-
No aesthetic injectables or body contouring treatments will ever be offered to under-18s.
-
Only Mesoestetic Blemiderm chemical peels are available for active acne or post-acne scarring in patients aged 13–17, following appropriate assessment and consent.
-
All patients under 18 are regarded as vulnerable and safeguarded under statutory guidance.
4. Initial Consultation Protocol
4.1 Mandatory Parent/Guardian Attendance
-
A parent or legal guardian must be physically present at the initial consultation.
-
The guardian must co-sign all consent forms and provide any additional safeguarding information relevant to the patient.
-
ID verification of both the patient and guardian must be completed and recorded in Insync Consent or equivalent.
4.2 Safeguarding Checks
-
The practitioner must assess for any signs of safeguarding concern, neglect, abuse, coercion, or psychological distress.
-
Where concern exists, the consultation should be paused and escalated to the clinic’s Named Safeguarding Lead (see Section 7).
4.3 Gillick Competence Assessment
-
Where appropriate, the practitioner will assess and document the young person’s ability to understand, weigh, and retain treatment information and make an informed decision.
-
If Gillick competence is not clearly established, the parent/guardian must remain involved in all future decision-making.
-
If Gillick competence is confirmed and documented, the patient may attend follow-ups alone, with the option of parental re-involvement at any time.
5. Follow-Up Consultation Protocol
5.1 Solo Attendance (Where Gillick Competence is Documented)
-
Patients may attend alone for follow-up or review consultations only if Gillick competence has been formally recorded at the initial appointment.
-
Practitioners must still assess capacity and understanding at each visit.
-
Written notes must confirm the young person’s ongoing ability to provide informed consent independently.
5.2 Circumstances Requiring Guardian Re-involvement
-
Where any of the following arise, the parent/guardian must be re-involved:
-
New treatment plan or change in clinical protocol
-
Emergence of safeguarding concerns
-
Patient revokes consent or appears confused/distressed
-
Inability to communicate effectively in English without assistance
-
6. Documentation Requirements
All under-18 consultations must include:
-
Copy of patient and guardian ID stored securely
-
Gillick Competence Form (template available) – ticked and signed
-
Consent forms co-signed (initial) or solo-signed (follow-ups only)
-
Safeguarding section on clinical note template completed
-
Any disclosures logged and escalated appropriately
7. Safeguarding & Escalation Pathways
-
Named Safeguarding Lead: Owen Dickinson (Managing Director)
-
Deputy Lead: Appointed Nurse Prescriber (as per staff file)
-
Referral Pathways: Local Safeguarding Children Board (LSCB) Derbyshire
Any disclosure of:
-
Emotional, physical, or sexual abuse
-
Neglect or exploitation
-
Forced medical decisions
-
Threats to the safety of the patient or others
…must be escalated immediately to the Designated Safeguarding Lead and recorded in a Safeguarding Concern Form.
8. Training Requirements
-
All staff involved with under-18s must complete:
-
Level 2 Safeguarding Children training
-
Annual refreshers via eLearning or in-clinic CPD
-
Internal briefing on this protocol
-
9. Policy Review
This protocol will be reviewed:
-
Annually
-
Following any safeguarding incident
-
Upon changes to CQC or legislative requirements
-
When offering any new treatments to under-18s
Signed:
Owen Dickinson
Managing Director & Safeguarding Lead
Date: 1st April 2025
